Rotator Cuff Repair
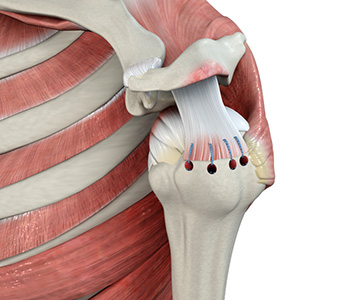
Rotator cuff is the group of tendons in the shoulder joint providing support and enabling wider range of motion. Major injury to these tendons may result in tear of these tendons and the condition is called as rotator cuff tear. It is one of the most common causes of shoulder pain in middle aged adults and older individuals. It may occur with repeated use of arm for overhead activities, while playing sports or during motor accidents. Rotator cuff tear causes severe pain, weakness of the arm, and crackling sensation on moving shoulder in certain positions. There may be stiffness, swelling, loss of movements, and tenderness in the front of the shoulder.
Rotator cuff tear is best viewed on magnetic resonance imaging. Symptomatic relief may be obtained with conservative treatments – rest, shoulder sling, pain medications, steroidal injections and certain exercises. However, surgery is required to fix the tendon back to the shoulder bone.
Surgery to repair the rotator cuff has traditionally been done through a large shoulder incision, about 6-10cm long, and the muscle over the rotator cuff was separated. Newer, advanced surgical techniques have been developed to minimize pain and recovery time. Arthroscopic rotator cuff repair is a minimally invasive surgery performed through tiny incisions, about 1 cm each, with an arthroscope.
The arthroscope is a small fibre-optic viewing instrument made up of a tiny lens, light source and video camera. The surgical instruments used in arthroscopic surgery are very small (only 3 or 4 mm in diameter) but appear much larger when viewed through an arthroscope.
The television camera attached to the arthroscope displays the image of the joint on a television screen, allowing the surgeon to look throughout the shoulder-at cartilage, ligaments, and the rotator cuff. The surgeon can determine the amount or type of injury, and then repair or correct the problem.
The benefits of arthroscopy compared to the alternative, open shoulder surgery, include:
- Smaller incisions
- Minimal soft tissue trauma
- Less pain
- Faster healing time
- Lower infection rate
- Less scarring
- Earlier mobilization
- Usually performed as outpatient day surgery
Rotator Cuff Repair with Surgery: 15-Year Outlook
Randomized Control Trial: JBJS American . 2024 Oct 2;106(19):1785-1796. doi: 10.2106/JBJS.24.00065.
Fifteen-Year Results of a Comparative Analysis of Tendon Repair Versus Physiotherapy for Small-to-Medium-Sized Rotator Cuff Tears: A Concise Follow-up of Previous Reports.
S Moosmayer [1] , G Lund [2] et al : PMID: 39197154 : PMCID: PMC11594065 : [3] DOI: 10.2106/JBJS.24.00065 [4]
After 15 years, rotator cuff repair generally shows durable, significantly improved function and reduced pain compared to pre-surgery, with many patients doing well, though some face issues like stiffness, re-tears, or arthritis, with success often linked to initial tear size and patient factors. Study confirm long-term satisfaction, but highlight that while most repairs stay intact, factors like older age, larger tears, and female sex can predict lower scores or need for revision surgery, with primary repair often superior to physiotherapy alone for long-term results.
Positive Long-Term Outcomes
- Long-Term Pain Relief: Most patients maintain significant pain
reduction and improved shoulder function for 15+ years [2, 3]. * High Satisfaction: Approximately 85-90% of patients report being satisfied with their results a decade and a half after surgery [1, 4]. * Structural vs. Functional Success: While some shoulders may develop “re-tears” or wear over 15 years, many patients do not feel a difference and continue to function well regardless of what an MRI might show [3, 4]. * The “5-Year” Rule: If your shoulder is stable and functional 5 years after surgery, it is highly likely to remain that way at the 15-year mark [2]. * Revision is Rare: Very few patients (typically less than 10%) require a second “redo” surgery within this 15-year window [4].
Factors Influencing my Results
- Tear Size Matters: Smaller initial tears are linked to better
long-term outcomes. * Age & Sex: Older age and female sex can be associated with lower scores (SAS, PROMIS-UE) and potentially worse results. * SMOKING / VAPING / Alcohol excess- If patient stops vaping/ smoking prior to operation , it leads to better outcomes. Smoking/ vaping/ Alcohol excess history leads to adverse outcomes. * Co-morbidities: More medical issues and Alcohol excess can lead to worse long-term outcomes.
Potential Long-Term Issues
- Re-tears & Failure: Some repairs fail to heal or re-tear, especially
patients with severe initial tears, who Vape or smoke , alcohol excess, significant comorbidities, though satisfactory results are still possible. * Ongoing Problems: Stiffness, weakness, ongoing pain, and eventual arthritis can still develop.
Key Message: Surgery provides lasting improvements in quality of life for most patients; success isn’t guaranteed for everyone. While the shoulder ages naturally, the functional benefits of the initial repair remain largely intact for most patients.
Actionable Resources:
* Review recovery expectations via the AAOS Patient Education Portal.