Arthritis Surgery for Thumb & Digits
Arthritis is an inflammatory condition of joints. There are several types of arthritis; the most common type is osteoarthritis or wear-and-tear arthritis that affects the joint at the base of the thumb. Thumb arthritis is more common in women than men, and usually occurs after the age of 40 years. Patients who have arthritis of the fingers may have swelling, pain, stiffness, and malformation all of which interfere with use of the hand.
Your doctor can usually make the diagnosis of thumb arthritis by examining the thumb. X-rays of the joint may be taken to know the severity of the disease and to determine any bone spurs or calcium deposits.
Nonsurgical treatment methods for relieving pain in an arthritic joint include activity modification, pain medications, and use of splints, and steroid injections. Surgery is usually considered if nonsurgical treatment fails to give relief. There are different surgical procedures that can be used and may include:
Synovectomy: This surgery is usually indicated for early cases of inflammatory arthritis where there is significant swelling (synovitis) that is causing pain or is limiting the range of motion of digits and thumb. Synovectomy is a surgical removal of the inflamed synovium (tissue lining the joint). The procedure may be performed using arthroscopy.
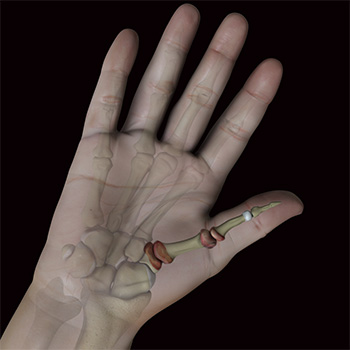
Arthroplasty: In this procedure, your surgeon removes the affected joint and replaces it with an artificial implant. In patients with post-traumatic arthritis and osteoarthritis where the bone is hard and demand on the hand is moderate, new ceramic implants are used. These are not desirable to use for severely damaged or unstable joint. In patients with inflammatory arthritis where the bone is not strong enough and the demand on the hand is low, older silicone rubber joints are generally used. These can be used for more severe joint damage and instable joint.
Arthrodesis: A fusion, also called an arthrodesis involves removal of the joints and fusing the bones of the joint together using metal wires or screws. Even though this surgery eliminates all motion at the base of the thumb, the resulting fusion is very hard.
This surgery is usually indicated when the joints are severely damaged, when there is limited mobility, damage to the surrounding ligaments and tendons, failed previous arthroplasty, and when heavy manual use is expected.
Your surgeon will discuss the options and help you decide which type of surgery is the most appropriate for you.
Rehabilitation
Following surgery, a rehabilitation program, often involving a physical therapist may help to regain hand strength and movement. You may need to use a post-operative splint for a while after surgery that helps to protect the hand while it heals. You may need to restrict activities for a minimum of 12 weeks to let the joint reconstruction heal properly. Although recovery is slow, you should be able to resume your normal activities within few months of surgery.
EVIDENCE
From: Hand Surgery Evidence updates: Jan 2026
Joint replacement versus trapeziectomy for trapeziometacarpal osteoarthritis: A systematic review. [6]
Datta S, Bandyopadhyay B, Tahir M, Shah R, Baid M, Hussain MW, Subbaraman K.
Cureus. 2025 Oct 19;17(10):e94908. doi: 10.7759/cureus.94908. eCollection 2025 Oct.
PMID: 41262787. Free PMC article. Review.
“Summary of findings: 11 studies, including retrospective and prospective cohort studies, a randomised controlled trial, and a same-patient comparison study, were analysed. Outcomes assessed included pain relief, grip and pinch strength, range of motion (ROM), patient-reported outcome measures (PROMs), recovery time, and complication rates. Both procedures effectively relieve pain and improve function. Joint replacement demonstrated superior short-term functional outcomes and faster recovery, particularly in strength restoration. However, it was associated with implant-specific complications. Trapeziectomy, while slower in recovery, showed consistent long-term efficacy and fewer implant-related issues. Both surgical options are viable. The choice should be individualised based on patient goals, anatomical considerations, and the balance between rapid functional recovery and implant-related risks.
However, I would like to clarify that my current scope of practice includes Thumb CMC joint excision- removal of bone- (trapeziectomy) only, and does NOT include Thumb CMC joint or any finger joint replacement surgery.